Germany’s healthcare system is one of the most advanced and efficient in the world, offering a blend of comprehensive coverage, high-quality care, and a well-structured funding model.
Designed to meet the needs of its diverse population, the system combines public and private elements to ensure access and equity.
While it has its complexities, its focus on affordability, accessibility, and innovation makes it a benchmark for other nations.
This article provides a clear and straightforward explanation of how the system operates, its costs, and the benefits it provides to those living in Germany.
Overview of the German Healthcare System
The German healthcare system is one of the most comprehensive and efficient in the world. Its foundations lie in principles of solidarity and universality, ensuring that all citizens and residents have access to necessary medical services.
Origins and Evolution
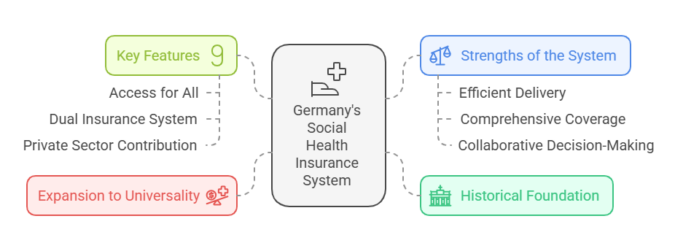
- Historical Foundation: Germany pioneered the concept of social health insurance in 1883 under Chancellor Otto von Bismarck.
- Expansion to Universality: Over time, the system evolved to include all citizens, mandating health insurance coverage in 2007.
Key Features
- Access for All: Everyone, regardless of income or health status, has access to healthcare services.
- Dual Insurance System: Statutory Health Insurance (SHI) and Private Health Insurance (PHI) cater to different income groups and needs.
- Private Sector Contribution: Experts for private insurance, such as those at audelio.de, provide tailored solutions for individuals seeking additional or alternative coverage.
Strengths of the System
- Efficient Delivery: Germany offers a seamless network of hospitals, outpatient clinics, and specialized medical centers.
- Comprehensive Coverage: Services include preventive care, inpatient and outpatient treatment, maternity benefits, and long-term care.
- Collaborative Decision-Making: The Federal Joint Committee ensures representation of insurers, providers, and patient advocates.
Challenges and Criticisms
- Rising costs of healthcare services.
- Increasing demand for elderly care due to demographic changes.
- Regional disparities in healthcare access.
Structure and Organization
The system is built on a foundation of statutory and private insurance, supported by government regulations and self-regulated professional bodies.
Statutory Health Insurance (SHI)
Statutory Health Insurance covers most of the population, with enrollment required for individuals earning below a specified income threshold (EUR 66,600 as of 2024). Premiums are calculated as a percentage of income, shared equally between employers and employees.
Family members without an independent income are covered at no extra cost. SHI funds are pooled and redistributed to ensure fair access to healthcare services, regardless of an individual’s financial status.
Private Health Insurance (PHI)
Private Health Insurance is an option for high-income earners, self-employed individuals, and civil servants. Premiums are determined by age, health risk, and selected benefits. Those opting for PHI often gain access to additional services, such as private hospital rooms and shorter waiting periods for treatments.
Unlike SHI, PHI policies are based on individual contracts, which offer more flexibility but can lead to higher costs in some cases.
Government Oversight and Decentralization
Germany’s federal government sets the legal framework for healthcare, while state governments oversee hospital capacity and public health services.
The Federal Joint Committee defines which treatments are included in SHI coverage, ensuring consistent service quality across the country.
Key Features of Care Delivery
- Outpatient Care: Primarily provided by office-based general practitioners (GPs) and specialists. Patients have free choice among providers without needing a referral in most cases.
- Inpatient Care: Delivered in hospitals, which may be publicly owned, private non-profit, or private for-profit institutions. Salaried physicians manage treatment for all insurance types.
Services and Benefits Covered
The structure ensures that statutory and private insurance both provide a wide array of essential and supplementary services.
Core Services Under Statutory Health Insurance (SHI)
SHI provides coverage for services deemed medically necessary, which include:
- Preventive Care: Regular check-ups, immunizations, cancer screenings, and child health exams.
- Outpatient and Inpatient Care: General practitioners, specialists, and hospital services are included.
- Mental Health Support: Counseling, therapy, and psychiatric care.
- Prescription Medications: Coverage excludes only lifestyle-related drugs.
- Maternity and Family Services: Prenatal care, childbirth support, and family counseling.
Additional Benefits Available in Private Health Insurance (PHI)
- Private hospital rooms and quicker access to specialists.
- Expanded dental and vision care.
- Alternative therapies, depending on the insurer’s offerings.
Sick Leave and Compensation
SHI also includes compensation for lost wages due to illness, covering up to 70% of income for a specified duration, with extensions possible in severe cases.
Specialized Long-Term Care
Germany has a mandatory, separate Long-Term Care Insurance (LTCI) system. LTCI provides benefits for individuals needing assistance due to age, illness, or disability.
- Home care by professional providers or family members.
- Full or partial residential nursing home care.
- Support for hospice and palliative care needs.
Funding and Cost Distribution
The system operates on a dual funding model, combining statutory contributions with private insurance premiums to ensure both sustainability and accessibility.
Statutory Health Insurance Contributions
- Premium Rates: Set at 14.6% of gross income, shared equally by employers and employees.
- Supplementary Contribution: An average of 1.3% is added, determined by each sickness fund.
- Dependents: Non-earning spouses and children are covered without additional cost.
Private Health Insurance Premiums
PHI premiums are calculated based on:
- Age and health risk at the time of enrollment.
- Level of benefits selected.
Unlike SHI, premiums are not linked to income and are paid entirely by the insured or their employer in part.
Government and Tax Funding
The government contributes to public health infrastructure, medical research, and hospital investments, ensuring the system remains robust and well-equipped.
Out-of-Pocket Expenses
- Copayments for hospital stays and prescription medications.
- Fees for services outside the SHI benefit package, often reimbursed by supplementary private insurance.
- Safety nets exist to cap out-of-pocket expenses for low-income individuals and families.
Quality Assurance and Performance Monitoring

Comprehensive oversight ensures that patients receive effective and safe medical services.
Federal Joint Committee and Standards
- Defining services covered under SHI.
- Setting quality benchmarks for providers.
- Conducting technology assessments to evaluate cost-effectiveness.
Hospital and Provider Quality Audits
The Institute for Quality Assurance and Transparency in Healthcare (IQTiG) monitors hospital performance through:
- Outcome indicators for key treatments.
- Annual quality reports published for public reference.
Continuous Professional Development
Physicians and doctors must meet ongoing education requirements to maintain their licenses. This ensures they stay updated with the latest medical advancements and practices.
Complaint and Arbitration Systems
Patients can report concerns to complaint management systems or arbitration boards, which handle malpractice claims and service deficiencies.
Disease Management Programs
Programs targeting chronic illnesses like diabetes and heart disease enhance care coordination.
- Evidence-based treatment plans.
- Data documentation and monitoring for quality assurance.
- Integration of Public and Private Healthcare Providers
- Both statutory and private insurance holders receive care from the same network of hospitals, clinics, and medical professionals.
Shared Access to Providers
Public and private patients are treated by the same healthcare professionals and facilities. This approach ensures:
- Uniform standards of care, regardless of insurance type.
- Flexibility for patients to choose among public, private, or nonprofit hospitals.
Role of Private Providers
Private hospitals and clinics have grown in prominence, often offering specialized or expedited services.
Cost Control and Sustainability Strategies
Germany employs several mechanisms to ensure the healthcare system remains financially sustainable while maintaining high standards of care.
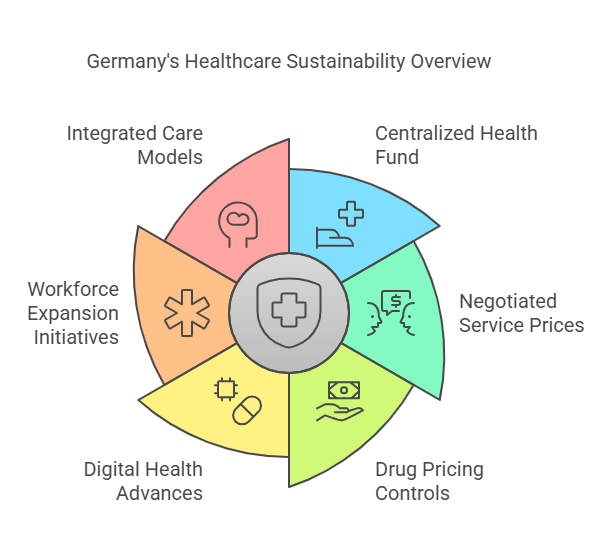
Centralized Health Fund
All contributions from statutory health insurance are pooled in a centralized health fund. This fund redistributes resources to sickness funds based on a risk-adjusted formula that considers:
- Age and sex of enrollees.
- Prevalence of chronic conditions.
Negotiated Service Prices
- Healthcare services are priced through negotiations between sickness funds, provider associations, and government agencies. This includes:
- Diagnosis-related group (DRG) payments for hospitals.
- Uniform fee schedules for outpatient care.
Drug Pricing Controls
Germany regulates pharmaceutical costs by:
- Requiring manufacturers to prove added benefit for new drugs.
- Setting reference prices and negotiating discounts with insurers.
- Policies promote efficiency by linking funding to quality outcomes. For example, hospitals receive financial incentives for reducing readmissions and delivering higher-quality care.
- Recent Innovations and Reforms: Germany’s healthcare system continues to evolve, with recent reforms addressing modern challenges and leveraging technology to improve care delivery.
Digital Health Advances
- Electronic health cards that store insurance and medical information.
- Implementation of digital prescription systems to streamline medication access.
- Telemedicine services that connect patients to specialists, particularly in rural areas.
Workforce Expansion Initiatives
Recognizing the strain on healthcare workers, the government has introduced measures to:
- Increase the number of trained nurses and physicians.
- Improve working conditions and salaries for medical staff.
Integrated Care Models
Efforts to enhance care coordination include:
- Disease management programs targeting diabetes, heart disease, and other chronic conditions.
- Pilot programs in rural regions that test integrated care networks combining outpatient, inpatient, and rehabilitative services.
- Germany is preparing for an aging population by expanding long-term care infrastructure and funding. Innovative programs encourage family caregiving while offering professional support through long-term care insurance.
Ensuring Quality of Care in Germany
Germany’s healthcare system prioritizes quality through mandatory standards, evaluations, and transparency in care delivery.
Federal Oversight and Regulation
- Defining the benefits covered by statutory health insurance.
- Developing quality assurance guidelines for providers.
- Overseeing health technology assessments for new treatments.
Hospital Quality Measures
Hospitals are required to report on selected quality indicators, which are published for public access. These indicators include:
- Surgical outcomes.
- Patient safety measures.
- Infection control protocols.
Provider Accountability
Physicians must adhere to strict professional regulations, participate in ongoing education, and follow evidence-based guidelines. Additionally, complaint management systems in hospitals and arbitration boards for medical malpractice claims ensure accountability.
Independent Quality Monitoring
Institutes like IQTiG (Institute for Quality Assurance and Transparency) evaluate and report on healthcare performance, ensuring that care delivery aligns with national standards.
FAQs
Are alternative treatments like acupuncture covered under German health insurance?
Statutory health insurance covers alternative treatments, including acupuncture, only for specific conditions such as chronic lower back pain or knee osteoarthritis. Private insurance plans may offer broader coverage for alternative therapies, depending on the policy.
What happens if someone cannot afford private health insurance premiums?
Individuals facing financial difficulties may remain in the statutory health system, which adjusts premiums based on income. For those in private insurance, mechanisms like aging reserves and capped rates for essential benefits help manage long-term affordability.
How is mental health care integrated into the healthcare system?
Germany offers mental health care through office-based psychiatrists, psychotherapists, and specialized hospital departments. Sickness funds cover services like psychotherapy and medication. Patients can directly seek help without referrals, ensuring easier access to care.
Are refugees and undocumented individuals eligible for healthcare in Germany?
Refugees and undocumented individuals are entitled to basic healthcare services for acute illnesses, pain, pregnancy, and childbirth. Social security funds cover these costs, ensuring access to essential treatments.
Does Germany’s healthcare system include dental care?
Statutory health insurance covers essential dental care, including routine check-ups, fillings, and basic prosthetics. More advanced or cosmetic treatments often require out-of-pocket payment or additional private insurance coverage.
The Bottom Line
Germany’s healthcare system stands out as a model of universal access, balancing public and private insurance options while maintaining high-quality care. Its emphasis on solidarity ensures that all residents, regardless of income or status, can access essential medical services. Challenges like rising costs and regional disparities persist, but ongoing reforms aim to improve efficiency, care coordination, and digital integration.